- What is MRI?
- How does MRI work?
- What is MRI used for?
- Are there risks?
- What are examples of NIBIB-funded projects in MRI?
What is MRI?
Magnetic Resonance Imaging (MRI) is a non-invasive imaging technology that produces three dimensional detailed anatomical images. It is often used for disease detection, diagnosis, and treatment monitoring. It is based on sophisticated technology that excites and detects the change in the direction of the rotational axis of protons found in the water that makes up living tissues.
How does MRI work?

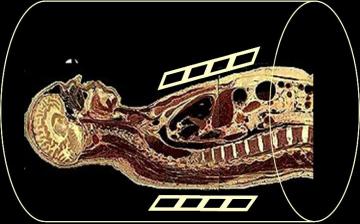
MRIs employ powerful magnets which produce a strong magnetic field that forces protons in the body to align with that field. When a radiofrequency current is then pulsed through the patient, the protons are stimulated, and spin out of equilibrium, straining against the pull of the magnetic field. When the radiofrequency field is turned off, the MRI sensors are able to detect the energy released as the protons realign with the magnetic field. The time it takes for the protons to realign with the magnetic field, as well as the amount of energy released, changes depending on the environment and the chemical nature of the molecules. Physicians are able to tell the difference between various types of tissues based on these magnetic properties.
To obtain an MRI image, a patient is placed inside a large magnet and must remain very still during the imaging process in order not to blur the image. Contrast agents (often containing the element Gadolinium) may be given to a patient intravenously before or during the MRI to increase the speed at which protons realign with the magnetic field. The faster the protons realign, the brighter the image.
What is MRI used for?
MRI scanners are particularly well suited to image the non-bony parts or soft tissues of the body. They differ from computed tomography (CT), in that they do not use the damaging ionizing radiation of x-rays. The brain, spinal cord and nerves, as well as muscles, ligaments, and tendons are seen much more clearly with MRI than with regular x-rays and CT; for this reason MRI is often used to image knee and shoulder injuries.
In the brain, MRI can differentiate between white matter and grey matter and can also be used to diagnose aneurysms and tumors. Because MRI does not use x-rays or other radiation, it is the imaging modality of choice when frequent imaging is required for diagnosis or therapy, especially in the brain. However, MRI is more expensive than x-ray imaging or CT scanning.
One kind of specialized MRI is functional Magnetic Resonance Imaging (fMRI.) This is used to observe brain structures and determine which areas of the brain “activate” (consume more oxygen) during various cognitive tasks. It is used to advance the understanding of brain organization and offers a potential new standard for assessing neurological status and neurosurgical risk.
Are there risks?
Although MRI does not emit the ionizing radiation that is found in x-ray and CT imaging, it does employ a strong magnetic field. The magnetic field extends beyond the machine and exerts very powerful forces on objects of iron, some steels, and other magnetizable objects; it is strong enough to fling a wheelchair across the room. Patients should notify their physicians of any form of medical or implant prior to an MR scan.
When having an MRI scan, the following should be taken into consideration:
- People with implants, particularly those containing iron, — pacemakers, vagus nerve stimulators, implantable cardioverter- defibrillators, loop recorders, insulin pumps, cochlear implants, deep brain stimulators, and capsules from capsule endoscopy should not enter an MRI machine.
- Noise—loud noise commonly referred to as clicking and beeping, as well as sound intensity up to 120 decibels in certain MR scanners, may require special ear protection.
- Nerve Stimulation—a twitching sensation sometimes results from the rapidly switched fields in the MRI.
- Contrast agents—patients with severe renal failure who require dialysis may risk a rare but serious illness called nephrogenic systemic fibrosis that may be linked to the use of certain gadolinium-containing agents, such as gadodiamide and others. Although a causal link has not been established, current guidelines in the United States recommend that dialysis patients should only receive gadolinium agents when essential, and that dialysis should be performed as soon as possible after the scan to remove the agent from the body promptly.
- Pregnancy—while no effects have been demonstrated on the fetus, it is recommended that MRI scans be avoided as a precaution especially in the first trimester of pregnancy when the fetus’ organs are being formed and contrast agents, if used, could enter the fetal bloodstream.
- Claustrophobia—people with even mild claustrophobia may find it difficult to tolerate long scan times inside the machine. Familiarization with the machine and process, as well as visualization techniques, sedation, and anesthesia provide patients with mechanisms to overcome their discomfort. Additional coping mechanisms include listening to music or watching a video or movie, closing or covering the eyes, and holding a panic button. The open MRI is a machine that is open on the sides rather than a tube closed at one end, so it does not fully surround the patient. It was developed to accommodate the needs of patients who are uncomfortable with the narrow tunnel and noises of the traditional MRI and for patients whose size or weight make the traditional MRI impractical. Newer open MRI technology provides high quality images for many but not all types of examinations.
What are examples of NIBIB-funded projects in MRI?
Replacing Biopsies with Sound
Chronic liver disease and cirrhosis affect more than 5.5 million people in the United States. NIBIB-funded researchers have developed a method to turn sound waves into images of the liver, which provides a new non-invasive, pain-free approach to find tumors or tissue damaged by liver disease. The Magnetic Resonance Elastography (MRE) device is placed over the liver of the patient before he enters the MRI machine. It then pulses sound waves through the liver, which the MRI is able to detect and use to determine the density and health of the liver tissue. This technique is safer and more comfortable for the patient as well as being less expensive than a traditional biopsy. Since MRE is able to recognize very slight differences in tissue density, there is the potential that it could also be used to detect cancer.
New MRI just for Kids
MRI is potentially one of the best imaging modalities for children since unlike CT, it does not have any ionizing radiation that could potentially be harmful. However, one of the most difficult challenges that MRI technicians face is obtaining a clear image, especially when the patient is a child or has some kind of ailment that prevents them from staying still for extended periods of time. As a result, many young children require anesthesia, which increases the health risk for the patient. NIBIB is funding research that is attempting to develop a robust pediatric body MRI. By creating a pediatric coil made specifically for smaller bodies, the image can be rendered more clearly and quickly and will demand less MR operator skill. This will make MRIs cheaper, safer, and more available to children. The faster imaging and motion compensation could also potentially benefit adult patients as well.
Another NIBIB-funded researcher is trying to solve this problem from a different angle. He is developing a motion correction system that could greatly improve image quality for MR exams. Researchers are developing an optical tracking system that would be able to match and adapt the MRI pulses to changes in the patient’s pose in real time. This improvement could reduce cost (since less repeat MR exams will have to take place due to poor quality) as well as make MRI a viable option for many patients who are unable to remain still for the exam and reduce the amount of anesthesia used for MR exams.
Determining the aggressiveness of a tumor
Traditional MRI, unlike PET or SPECT, cannot measure metabolic rates. However, researchers funded by NIBIB have discovered a way to inject specialized compounds (hyperpolarized carbon 13) into prostate cancer patients to measure the metabolic rate of a tumor. This information can provide a fast and accurate picture of the tumor’s aggressiveness. Monitoring disease progression can improve risk prediction, which is critical for prostate cancer patients who often adopt a wait and watch approach.